More than 100,000 people have been infected with a new coronavirus that has spread widely from its origin in China over the past few months. More than 3,000 have already died. Our comprehensive guide for understanding and navigating this global public health threat is below.
This is a rapidly developing epidemic, and we will update this guide regularly to keep you as prepared and informed as possible.
March 8: Initial publication of the document.
Table of Contents
- How worried should I be?
- What is SARS-CoV-2?
- Where did SARS-CoV-2 come from?
- How did it start infecting people?
- What happens when youre infected with SARS-CoV-2?
- What are the symptoms?
- How severe is the infection?
- Who is most at risk of getting critically ill and dying?
- Are men more at risk?
- Are children less at risk?
- How long does COVID-19 last?
- How many people die from the infection?
- How does COVID-19 compare with seasonal flu in terms of symptoms and deaths?
- How does SARS-CoV-2 spread?
- How does coronavirus transmission compare with flu?
- How likely am I to get it in normal life?
- What can I do to prevent spread and protect myself?
- Should I get a flu vaccine?
- When, if ever, should I buy or use a face mask?
- Should I avoid large gatherings and travel?
- What precautions should I take if I do travel?
- How should I prepare for the worst-case scenario?
- Should I keep anything in my medicine cabinet for COVID-19?
- Should I go to a doctor if I think I have COVID-19?
- When should I seek emergency care?
- Is the US healthcare system ready for this?
- What are the problems with testing in the US?
- What could happen if healthcare facilities become overwhelmed?
- When will all of this be over in the US?
- Will SARS-CoV-2 die down in the summer?
- Will it become a seasonal infection?
- What about treatments and vaccines?
How worried should I be?
You should be concerned and take this seriously. But you should not panic.
This is the mantra public health experts have adopted since the epidemic mushroomed in January—and its about as comforting as it is easy to accomplish. But its important that we all try.
This new coronavirus—dubbed SARS-CoV-2—is unquestionably dangerous. It causes a disease called COVID-19, which can be deadly, particularly for older people and those with underlying health conditions. While the death rate among infected people is unclear, even some current low estimates are seven-fold higher than the estimate for seasonal influenza.
And SARS-CoV-2 is here in the US, and it's circulating—we are only starting to determine where it is and how far it has spread. Problems with federal testing have delayed our ability to detect infections in travelers. And as we work to catch up, the virus has kept moving. It now appears to be spreading in several communities across the country. Its unclear if we will be able to get ahead of it and contain it; even if we can, it will take a lot of resources and effort to do it.
All that said, SARS-CoV-2 is not an existential threat. While it can be deadly, around 80 percent of cases are mild to moderate, and people recover within a week or two. Moreover, there are obvious, evidence-based actions we can take to protect ourselves, our loved ones, and our communities overall.
Now is not the time for panic, which will only get in the way of what you need to be doing. While its completely understandable to be worried, your best bet to getting through this unscathed is to channel that anxious energy into doing what you can to stop SARS-COV-2 from spreading.
And to do that, you first need to have the most complete, accurate information on the situation as you can. To that end, below is our best attempt to address all of the questions you might have about SARS-CoV-2, COVID-19, and the situation in the US.
Well start with where all of this starts—the virus itself.
What is SARS-CoV-2?
SARS-CoV-2 stands for severe acute respiratory syndrome coronavirus 2. As the name suggests, its a coronavirus and is related to the coronavirus that causes SARS (Severe Acute Respiratory Syndrome). Note: When SARS-CoV-2 was first identified it was provisionally dubbed 2019 novel coronavirus, or 2019-nCoV.
Coronaviruses are a large family of viruses that get their name from the halo of spiked proteins that adorn their outer surface, which resemble a crown (corona) under a microscope. As a family, they infect a wide range of animals, including humans.
With the discovery of SARS-CoV-2, there are now seven types of coronaviruses known to infect humans. Four regularly circulate in humans and mostly cause mild to moderate upper-respiratory tract infections—common colds, essentially.
The other three are coronaviruses that recently jumped from animal hosts to humans, resulting in more severe disease. These include SARS-CoV-2 as well as MERS-CoV, which causes Middle East Respiratory Syndrome (MERS), and SARS-CoV, which causes SARS.
In all three of these cases, the viruses are thought to have moved from bats—which have a large number of coronavirus strains circulating—to humans via an intermediate animal host. Researchers have linked SARS-CoV to viruses in bats, which may have moved to humans through masked palm civets and raccoon dogs sold for food in live-animal street markets in China. MERS is thought to have spread from bats to dromedary camels before jumping to humans.
Where did SARS-CoV-2 come from?
SARS-CoV-2 is related to coronaviruses in bats, but its intermediate animal host and route to humans are not yet clear. There has been plenty of speculation that the intermediate hose could be pangolins, but that is not confirmed.
How did it start infecting people?
While the identity of SARS-CoV-2s intermediate host remains unknown, researchers suspect the mystery animal was present in a live animal market in Wuhan, China—the capital city of Chinas central Hubei Province and the epicenter of the outbreak. The market, which was later described in Chinese state media reports as “filthy and messy,” sold a wide range of seafood and live animals, some wild. Many of the initial SARS-CoV-2 infections were linked to the market; in fact, many early cases were in people who worked there.
Public health experts suspect that the untidiness of the market could have led to the virus spread. Such markets are notorious for helping to launch new infectious diseases—they tend to cram humans together with a variety of live animals that have their own menageries of pathogens. Close quarters, meat preparation, and poor hygienic conditions all offer viruses an inordinate number of opportunities to recombine, mutate, and leap to new hosts, including humans
That said, a report in The Lancet describing 41 early cases in the outbreak indicates that the earliest identified person sickened with SARS-CoV-2 had no links to the market. As Ars has reported before, the case was in a man whose infection began causing symptoms on December 1, 2019. None of the mans family became ill, and he had no ties to any of the other cases in the outbreak.
The significance of this and the ultimate source of the outbreak remain unknown.
The market was shut down and sanitized by Chinese officials on January 1 as the outbreak began to pick up.
What happens when youre infected with SARS-CoV-2?
In people, SARS-CoV-2 causes a disease dubbed COVID-19 by the World Health Organization (WHO). As the US Centers for Disease Control and Prevention (CDC) points out, the CO stands for corona, VI for virus, and D for disease.
What are the symptoms?
COVID-19 is a disease with a range of symptoms and severities, and we are still learning about the full spectrum. So far, it seems to span from mild or potentially asymptomatic cases all the way to moderate pneumonia, severe pneumonia, respiratory distress, organ failure and, for some, death.
Many cases start out with fever, fatigue and mild respiratory symptoms, like a dry cough. Most cases dont get much worse, but some do progress into a serious illness.
According to data from nearly 56,000 laboratory-confirmed COVID-19 patients in China, the rundown of common symptoms went as follows:
- 88 percent had a fever
- 68 percent had a dry cough
- 38 percent had fatigue
- 33 percent coughed up phlegm
- 19 percent had shortness of breath
- 15 percent had joint or muscle pain
- 14 percent had a sore throat
- 14 percent headache
- 11 percent had chills
- 5 percent had nausea or vomiting
- 5 percent had nasal congestion
- 4 percent had diarrhea
- Less than one percent coughed up blood or blood-stained mucus
- Less than one percent had watery eyes
That data was published in a report by a band of international health experts assembled by the WHO and Chinese officials (called the WHO-China Joint mission), who toured the country for a few weeks in February to assess the outbreak and response efforts.
How severe is the infection?
Most people infected will have a mild illness and recover completely in two weeks.
In an epidemiological study of 44,672 confirmed cases in China, authored by an emergency response team of epidemiologists and published by the Chinese CDC, researchers reported that about 81 percent of cases were considered mild. The researchers defined mild cases as those ranging from the slightest symptoms to mild pneumonia. None of the mild cases were fatal; all recovered.
Of the remaining cases in the study, about 14 percent were considered severe, which was defined as cases with difficult or labored breathing, an increased rate of breathing, and decreased blood oxygen levels. None of the severe cases were fatal; all recovered.
Nearly 5 percent of cases were considered critical. These cases included respiratory failure, septic shock, and/or multiple organ dysfunction or failure. About half of these patients died.
Finally, 257 cases (0.6 percent) lacked severity data.
The overall fatality rate in the patients examined was 2.3 percent.
Who is most at risk of getting critically ill and dying?
Your risk of becoming severely ill and dying increases with age and underlying health conditions.
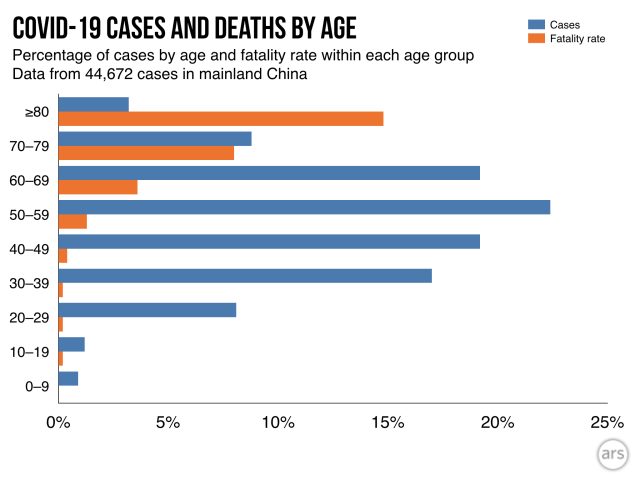
In the group of 44,672 cases discussed above, the highest fatality rates were among those aged 60 and above. People aged 60 to 69 had a fatality rate of 3.6 percent. The 70 to 79 age group had a fatality rate of about 8 percent, and those 80 or older had a fatality rate of nearly 15 percent.
Additionally, the researchers had information about other health conditions for 20,812 of the 44,672 patients. Of those with additional medical information available, 15,536 said they had no underlying health conditions. The fatality rate among that group was 0.9 percent.
The fatality rates were much higher among the remaining 5,279 patients who reported some underlying health conditions. Those who reported cardiovascular disease had a fatality rate of 10.5 percent. For patients with diabetes, the fatality rate was 7.3 percent. Patients with chronic respiratory disease had a rate of 6.3 percent. Patients with high blood pressure had a fatality rate of 6.0 percent and cancer patients had a rate of 5.6 percent.
Puzzlingly, men had a higher fatality rate than women. In the study, 2.8 percent of adult male patients died compared with a 1.7 percent fatality rate among female patients.
Are men more at risk?
In multiple studies, researchers have noted higher case numbers in men than in women. The WHO Joint Mission report found that men made up 51 percent of cases. Another study of 1,099 patients found that men made up 58 percent of cases.
So far, it is unclear if these numbers are real or if they would even out if researchers looked at larger numbers of cases. Its also unclear if this bias may reflect differences in exposure rates, underlying health conditions, or smoking rates that may make men more susceptible.
That said, sex differences have been seen in illnesses caused by SARS-CoV-2s relatives, SARS-CoV and MERS-CoV. There is some preliminary research looking into this in mice. Some findings suggest that there may be a protective effect from the activity of the female hormone estrogen. Other research has also suggested that genes found on the X chromosome that are involved in modulating immune responses to viruses may also serve to better protect genetically female people, who have two X chromosomes, compared with genetic males, who have only one X chromosome.
Are children less at risk?
Yes, it appears so. In all of the studies and data so far, children make up tiny fractions of the cases and have very few reported deaths. In the 44,672 cases examined by the Chinese CDC, less than one percent were in children ages 0 to 9 years old. None of those cases was fatal. Similar findings have been reported in other studies.
The WHO-China Joint Mission report also noted that children appear largely unscathed in this epidemic, writing, “disease in children appears to be relatively rare and mild.” From the data so far, they report that “infected children have largely been identified through contact tracing in households of adults.”
An unpublished, un-peer-reviewed study of 391 cases in Shenzhen, China, seems to support that observation. It noted that within households, children appeared just as likely to get infected as adults, but they had milder cases. The study was posted March 4 on a medical preprint server.
Still, as the Joint Mission report noted, given the data available, it is not possible to determine the extent of infection among children and what role that plays in driving the spread of disease and the epidemic overall. “Of note,” the report went on, “people interviewed by the Joint Mission Team could not recall episodes in which transmission occurred from a child to an adult.”
How long does COVID-19 last?
On average, it takes five to six days from the day you are infected with SARS-CoV-2 until you develop symptoms of COVID-19. This pre-symptomatic period—also known as "incubation"—can range from one to 14 days.
From there, those with mild disease tend to recover in about two weeks, while those with more severe cases can take three to six weeks to recover, according to WHO Director-General Dr. Tedros Adhanom Ghebreyesus, who goes by Dr. Tedros.
How many people die from the infection?
This is a difficult question to answer. The bottom line is that we dont really know.
Case fatality rates (CFR)—that is, the number of infected people who will die from the infection—are simply calculated by dividing the number of dead by the number of recovered plus dead. The CFRs youve probably seen so far have likely been a crude version of this: deaths divided by total cases.
One problem with these crude calculations is that the cases were counting arent all resolved. Some of the patients who are currently sick may later go on to die. In that situation, the patients' cases are counted, but their deaths are not (yet). This skews the current calculation to make the CFR look artificially low.
But a much larger concern is that we are undercounting the number of cases overall. Because most of the COVID-19 cases that we know about are mild, health experts suspect that many more infected people have not presented themselves to healthcare providers to be tested. They may have mistaken their COVID-19 case for a common cold or didnt notice it at all. In areas hard hit by COVID-19, there may not have been enough testing capacity to detect all of the mild cases. If a large number of mild cases are being missed in the total case count, it could make the CFR look artificially high.
The best way to clear up this uncertainty is to wait until one of the local outbreaks is completely over and then to do blood tests on the general population to see how many people were infected. Those blood tests would look for antibodies that target SARS-CoV-2. (Antibodies are Y-shaped proteins that the immune system makes to help identify and attack pathogens and other unfriendly invaders.) The presence of antibodies against a specific germ in a persons blood indicates that the person has been exposed to that germ, either through infection or immunization. Screening the general population for SARS-CoV-2 antibodies will give a clearer picture of how many people were actually infected—regardless of whether they were symptomatic or diagnosed while sick. That number can then be used to calculate an accurate CFR.
So far, some preliminary population screening for COVID-19 infections has been done in China, specifically in Guangdong province. Screening of 320,000 people who went to a fever clinic suggested that we may not be missing a vast number of mild cases. This in turn suggests that the CFRs we are calculating now are not wildly higher than they should be. However, experts still suspect that many mild cases are going unreported, and many still anticipate that the true CFR will be lower than what we are calculating now.
Beyond getting the basic number of cases and deaths right, CFRs are also tricky because they can vary by population, time, and place. Weve already noted above that the CFR increases in patient populations based on age, gender, and underlying health. But as time goes on, healthcare providers will get collectively better at identifying and treating patients, thereby lowering the CFR.
Complicating these statistics further, the quality of healthcare differs from place to place. The CFR in a resource-poor hospital may be higher than that in a resource-rich hospital. Additionally, health systems overwhelmed in an outbreak may not be able to provide optimal care for every patient, artificially increasing the CFR in those places.
This seems to be what weve seen in China so far. In the WHO-China Joint Mission report, the experts noted that in Wuhan—where the outbreak began and where health systems have been crushed by the number of cases—the CFR was a whopping 5.8 percent. The rest of China at the time had a CFR of 0.7 percent.
As of March 5, there were about 13,000 cases and 400 deaths reported outside of Chinas Hubei Province (where Wuhan is located). A crude calculation puts the CFR around 3 percent, but this calculation will likely drift throughout the outbreak. We will update the current crude CFR periodically.
How does COVID-19 compare with seasonal flu in terms of symptoms and deaths?
Most cases of COVID-19 are mild and may feel similar to the seasonal flu before a person recovers.
Though the case fatality rate is not yet clear for COVID-19 (as noted above), it so far appears to be significantly higher than the CFRs seen from seasonal flu in the US.
Overall CFRs for COVID-19 have hovered around 2 percent to 3 percent during the outbreak. As reported by Kaiser Health News, Christopher Mores, a global health professor at George Washington University, calculated the average 10-year mortality rate for flu in the US at 0.1 percent, based on CDC data. Many experts use this figure, including Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
Likewise, WHO Director-General Dr. Tedros noted in a recent statement that “seasonal flu generally kills far fewer than one percent of those infected.”
Still, a lower CFR doesnt mean a low death toll. So far this flu season, the CDC estimates that up to 45 million Americans have been infected, hospitalizing up to 560,000 and killing 46,000.
Influenza is a leading cause of death in the US.
How does SARS-CoV-2 spread?
SARS-CoV-2 spreads mainly in respiratory droplets—tiny, germ-toting globs that are launched from the mouth or nose when you breathe heavily, talk, cough, or sneeze. Published data suggests that a single sneeze can unleash 40,000 droplets between 0.5–12 micrometers in diameter. Once airborne, these fall rapidly onto the ground and typically dont land more than one meter away. SARS-CoV-2 does not linger in the air.
If any droplets containing SARS-CoV-2 land on a nearby person and gain access to the eyes, nose, or mouth—or are delivered there by a germy hand—that person can get infected.
If droplets containing SARS-CoV-2 land on surfaces, they can get picked up by others who can then contract the infection. According to epidemiologist Maria Van Kerkhove, an outbreak expert at the WHO, SARS-CoV-2 appears to be like its relative, SARS-CoV, in that surface contamination does seem to play a role in the epidemic.
It is unclear how long SARS-CoV-2 can survive on a surface. A recent review published in The Journal of Hospital Infection suggested that human-infecting coronaviruses in general may be able to survive on surfaces for up to nine days.
For now, the WHO says SARS-CoV-2 may survive on surfaces for anywhere from a few hours to several days. The organization notes that survival will depend on environmental factors, such as temperature, humidity, and the type of surface.
That said, as Dr. Van Kerkhove noted, SARS-CoV-2 is quickly killed by disinfecting agents. As the review of coronavirus surface survival reported, the viruses are “efficiently inactivated by surface disinfection procedures with 62–71 percent ethanol, 0.5 percent hydrogen peroxide, or 0.1 percent sodium hypochlorite (bleach) within 1 minute.”
Last, genetic material from SARS-CoV-2 does seem to be shed in some patients' feces—potentially in up to 30 percent of patients, according to the report by the WHO-China Joint Mission. A recent study in JAMA also found the virus lurking in toilet bowl and bathroom sink samples. “However,” as the Joint Mission report states, “the fecal-oral route does not appear to be a driver of COVID-19 transmission.” Moreover, routine bathroom cleaning efficiently eliminated the infectious threat, the authors of the JAMA article concluded.
How does coronavirus transmission compare with flu?
In a press briefing on March 3, WHO Director-General Dr. Tedros emphasized that “this virus is not SARS, its not MERS, and its not influenza. It is a unique virus with unique characteristics.”
“Both COVID-19 and influenza cause respiratory disease and spread the same way, via small droplets of fluid from the nose and mouth of someone who is sick,” he said. “However… COVID-19 does not transmit as efficiently as influenza, from the data we have so far. With influenza, people who are infected but not yet sick are major drivers of transmission, which does not appear to be the case for COVID-19.”
While media reports have widely circulated fears that asymptomatic people are silently spreading COVID-19 around communities and countries, there is little data to back that up. In fact, asymptomatic cases appear rare and potentially misclassified.
Dr. Tedros noted that only 1 percent of cases in China are reported as “asymptomatic.” And of that 1 percent, 75 percent do go on to develop symptoms.
For COVID-19, the data indicates that people coughing and sneezing are the biggest drivers of the spread of SARS-CoV-2. Moreover, the thrust of the epidemic in China has been from the spread of the virus through households and close contacts, not unconnected community members.
How likely am I to get it in normal life?
Your risk of exposure depends on where you live and where youve recently traveled. In the US, the virus is spreading in certain communities but is not thought to be circulating widely, according to the CDC. Unless there have been a number of cases reported in your area, your risk is considered low.
That said, with more testing happening, more cases will appear daily. There are basic things you can do to protect yourself and prepare for cases in your area.
What can I do to prevent spread and protect myself?
The most important things you can do to protect yourself from COVID-19 (as well as seasonal respiratory infections, like flu and cold) is to practice good, basic hygiene. That is:
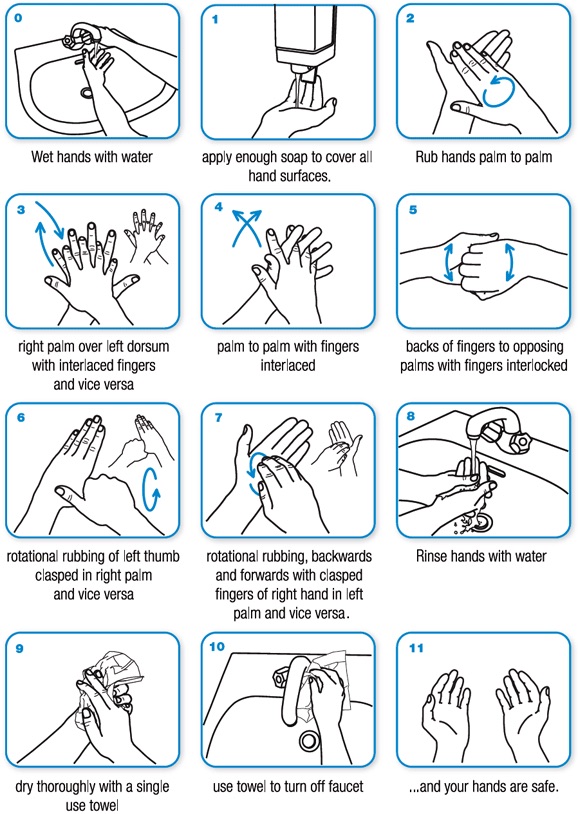
- Wash your hands frequently and thoroughly.
- Make sure you wash your hands with soap and water for 20 seconds—the time it takes you to hum the Happy Birthday song twice. (One clever Twitter user came up with some alternative tunes for your mitt-scrubbing pleasure.)
- You should especially wash your hands before eating, after using the restroom, sneezing, coughing, or blowing your nose.
- If you cant get to a sink, use a hand sanitizer that has at least 60 percent alcohol, the CDC says.
- Avoid touching your face, particularly your eyes, nose, and mouth.
- If you cough or sneeze, cover your face with your elbow or a tissue. If you use a tissue, throw that tissue away promptly, then go wash your hands.
- Avoid close contact with sick people. If you think someone has a respiratory infection, its safest to stay 2 meters away.
- If you are sick, try to stay home to get better and avoid spreading the infection.
- Regularly disinfect commonly touched surfaces and items in your house, such as door knobs and counter tops.
Should I get a flu vaccine?
YES. Getting a flu vaccine will protect you from the seasonal influenza and help prevent you from spreading that virus. Though the vaccine is not 100 percent effective, if you do still get sick with the flu after you are vaccinated, your illness will be milder than if you did not get vaccinated.
Getting a flu vaccine is something you should do every year to protect yourself and your community, including those most vulnerable to the infection and those who cannot get vaccinated for medical reasons. But, amid the COVID-19 epidemic, getting a flu shot is even more important.
COVID-19 can resemble the symptoms of influenza. If people are vaccinated against the flu and there are few cases of flu in an area, it may make spotting new COVID-19 cases easier. Moreover, healthcare systems around the country are already stretched thin by flu patients who need care and hospitalization each season. In this flu season so far, the CDC estimates that flu is responsible for up to 21 million medical visits and 560,000 hospitalizations.
Fewer flu patients means more healthcare resources can be directed to detect and treat COVID-19 cases and thwart the epidemic.
When, if ever, should I buy or use a face mask?
If you are not sick, do not buy a face mask. If you have one already and you are well, it is not recommended that you use it.
Face masks are now in short supply globally, and prices have surged. This is making it difficult for healthcare workers to get the supplies they need to keep themselves safe so they can stay healthy, keep treating patients, and avoid spreading the infection. This tragic situation is exacerbating the outbreak.
In a March 3 plea, the WHO called on industry and governments to step up production of masks and help thwart inappropriate buying.
“The World Health Organization has warned that severe and mounting disruption to the global supply of personal protective equipment (PPE)—caused by rising demand, panic buying, hoarding and misuse—is putting lives at risk from the new coronavirus and other infectious diseases,” the agency said in a statement.
“We cant stop COVID-19 without protecting health workers first,” WHO Director-General Dr. Tedros said.
In addition to putting healthcare workers at risk, wearing a mask may also put you at risk. For one thing, face masks are not entirely effective. Masks still leave your eyes exposed—if rubbed with germy hands, they can be an entry point for viruses. Surgical masks are loose-fitting and leave open the possibility of infectious particles working their way around the mouth. Even the use of N95 respirators, which are designed to protect against respiratory droplets, may not be that helpful to you, since they require proper fitting, and many people do not wear them correctly or consistently.
Some experts suggest that when members of the public wear face masks, they tend to fuss with them and touch their faces more. This increases the risk of transferring pathogens from hands to entry points. Also, if you touch the outside surface of a contaminated face mask, you can then contaminate your hand and go on to infect yourself. This negates the purpose of wearing a face mask.
Last, some health experts worry that wearing face masks may give people a false sense of security, potentially making them lax about other precautions and protections.
The only time experts recommend that members of the public wear a mask is if they are caring for a sick person or are already sick and showing signs of COVID-19. In that case, wearing a mask could reduce the risk that you will spread the infection to others.
Otherwise, masks should be reserved for healthcare workers.
Should I avoid large gatherings and travel?
Unfortunately, there is no clear or general answer to this. Like your risk of exposure generally, risk from attending events and traveling depend on where you are and where you are going.
Any time youre faced with such a dRead More – Source
[contf] [contfnew] 
arstechnica
[contfnewc] [contfnewc]







